When you bring a pet into your home, they become part of the family so naturally they need to be considered when you are planning a holiday. The first and maybe the biggest decision is whether or not they are coming with you!
Travelling WITH pets
Bringing your pet along on holidays can be so rewarding, but it does require some forward planning and some consideration both along the way AND at your final destination.
Never leave your pet unattended in the car.
Health check and grooming
Before you depart, bring your pet into the clinic for a health check and get them up-to-date with immunisations, medications and preventative health treatments. Some airlines or other transport carriers will require a ‘fit to travel’ certificate and/or vaccination certificate which can be provided after your pet’s check-up.
It’s common courtesy to fellow travellers to ensure your pet is clean and fresh smelling, so it’s also a great idea to book your pet in for professional grooming, or give them a good wash at home.
Phone ahead
Travelling with pets has become a lot easier in recent years, with transport, hotels, air bnbs and even campgrounds now offering pet-friendly facilities. Having said that… don’t assume! If you’re planning on taking your pet on holidays with you, please phone ahead to ensure your accommodation is pet-friendly. It doesn’t matter where you’re staying – the last thing you want to discover when you arrive is that your little buddy is not permitted on the premises!
Pack all the things
Don’t forget your pets’ needs in the packing frenzy! Dedicate a bag or suitcase just for your pet to ensure everything is within easy access, including a leash, toys, food, medications, treats, bowls and bedding. It’s a good idea to carry extra bottles of water to keep your pet hydrated along your journey.
List of contacts
In addition to the ‘stuff’, make sure you have your vet’s info handy so if anything were to happen, you can contact them quickly. Also take the time to research emergency vets in the area where you will be holidaying, and bring your pet insurance details with you just in case.
Travelling WITHOUT pets
Boarding Facilities
Boarding kennels and catteries book-out quickly, especially around peak times including school holidays so we advise planning well ahead book your pet into a reputable facility.
Boarding kennels and catteries house lots of animals within relatively small spaces. Some facilities will offer smaller rooms with one or two animals each, others house larger groups together. No matter which facility you choose, it’s important to discuss the space your pet will have access to, what your pet will be fed, your expectations around routine/exercise, any medication that needs to be administered and your pet’s temperament around other animals. All this information will help the staff ensure your pet gets the best possible care while you’re away.
Vaccinations
Reputable boarding kennels and catteries will require a copy of your pet’s vaccination history from your veterinarian. If they don’t ask it from you, chances are they will not be asking it from anyone else so there’s every chance that your pet will be exposed to illnesses at their facility. We recommend always selecting a facility that requires proof of pets’ vaccination histories.
Kennels and catteries will differ in the vaccinations they require their guests to be up-to-date with, but generally the minimum requirements are as follows:
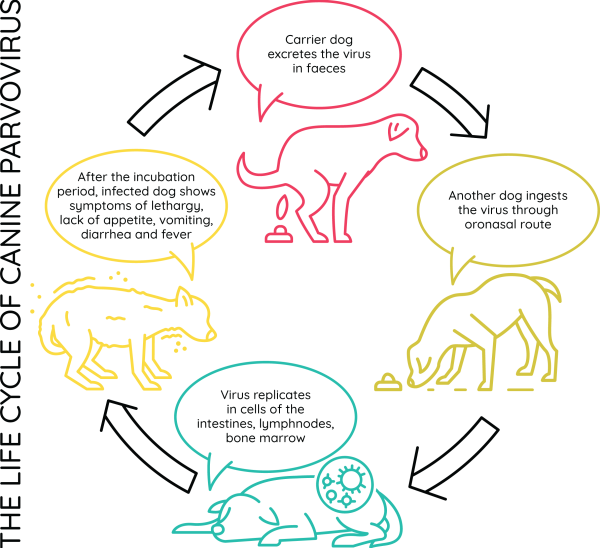
- Dogs will usually need a current C5 Vaccine to provide coverage for canine distemper virus, hepatitis, kennel cough, parainfluenza and parvovirus. While this vaccination is usually given to dogs when they’re puppies, booster vaccines are recommended to maintain immunity. Kennel cough is very common on the Sunshine Coast so please ensure your dog’s C5 is always up-to-date.
- Cats will usually need a current F3 Vaccine to provide coverage for herpesvirus, calicivirus and parvovirus. This vaccine should be administered annually, beginning from when you cat is a kitten.
It is also a good idea to be sure your pet receives up-to-date worming, flea and tick prevention prior to boarding.
IMPORTANT: Most vaccines require two weeks to become effective, so should be administered well-ahead of your travel plans.
House Sitters
Some pets have a very shy, or anti-social temperament and can easily become stressed when away from their home environment (cats in particular are quite territorial). These types of animals may be much happier with a house sitter staying in your home with them instead. The other great thing about house sitters is that they can sometimes be more economical and can also take care of multiple animals, including the smaller ones (guinea pigs, fish, birds etc) who are more difficult to find temporary accommodation for.
It’s technically very easy to find a house sitter through established websites however, there are important steps you need to take to find a pet sitter that is trustworthy and reliable. Always interview the person and make sure they understand your expectations. Obtain and check references to ensure you feel safe leaving someone in your home and in charge of your pet/s.
Safe travelling!